Clinical Signs and Symptoms of Influenza
submited by pub4world at Nov, 9, 2011 22:1 PM from CDC
2009-10 Influenza Prevention & Control Recommendations
Clinical Signs and Symptoms of Influenza
Diagnosis
Signs and Symptoms
Influenza viruses are spread from person to person primarily through large-particle respiratory droplet transmission (e.g., when an infected person coughs or sneezes near a susceptible person). Transmission via large-particle droplets requires close contact between source and recipient persons, because droplets do not remain suspended in the air and generally travel only a short distance (less than or equal to 1 meter) through the air. Contact with respiratory-droplet contaminated surfaces is another possible source of transmission. Airborne transmission (via small-particle residue [less than or equal to 5?m] of evaporated droplets that might remain suspended in the air for long periods of time) also is thought to be possible, although data supporting airborne transmission are limited. The typical incubation period for influenza is 1—4 days (average: 2 days). Adults shed influenza virus from the day before symptoms begin through 5—10 days after illness onset. However, the amount of virus shed, and presumably infectivity, decreases rapidly by 3—5 days after onset in an experimental human infection model. Young children also might shed virus several days before illness onset, and children can be infectious for 10 or more days after onset of symptoms. Severely immunocompromised persons can shed virus for weeks or months.
Uncomplicated influenza illness is characterized by the abrupt onset of constitutional and respiratory signs and symptoms (e.g., fever, myalgia, headache, malaise, nonproductive cough, sore throat, and rhinitis). Among children, otitis media, nausea, and vomiting also are commonly reported with influenza illness. Uncomplicated influenza illness typically resolves after 3—7 days for the majority of persons, although cough and malaise can persist for >2 weeks. However, influenza virus infections can cause primary influenza viral pneumonia; exacerbate underlying medical conditions (e.g., pulmonary or cardiac disease); lead to secondary bacterial pneumonia, sinusitis, or otitis media; or contribute to coinfections with other viral or bacterial pathogens. Young children with influenza virus infection might have initial symptoms mimicking bacterial sepsis with high fevers, and febrile seizures have been reported in 6%—20% of children hospitalized with influenza virus infection. Population-based studies among hospitalized children with laboratory-confirmed influenza have demonstrated that although the majority of hospitalizations are brief (2 or fewer days), 4%—11% of children hospitalized with laboratory-confirmed influenza required treatment in the intensive care unit, and 3% required mechanical ventilation. Among 1,308 hospitalized children in one study, 80% were aged <5 years, and 27% were aged <6 months. Influenza virus infection also has been uncommonly associated with encephalopathy, transverse myelitis, myositis, myocarditis, pericarditis, and Reye syndrome.
Respiratory illnesses caused by influenza virus infection are difficult to distinguish from illnesses caused by other respiratory pathogens on the basis of signs and symptoms alone. Sensitivity and predictive value of clinical definitions vary, depending on the prevalence of other respiratory pathogens and the level of influenza activity. Among generally healthy older adolescents and adults living in areas with confirmed influenza virus circulation, estimates of the positive predictive value of a simple clinical definition of influenza (acute onset of cough and fever) for laboratory-confirmed influenza infection have varied (range: 79%—88%).
Young children are less likely to report typical influenza symptoms (e.g., fever and cough). In studies conducted among children aged 5—12 years, the positive predictive value of fever and cough together was 71%—83%, compared with 64% among children aged <5 years. In one large, population-based surveillance study in which all children with fever or symptoms of acute respiratory tract infection were tested for influenza, 70% of hospitalized children aged <6 months with laboratory-confirmed influenza were reported to have fever and cough, compared with 91% of hospitalized children aged 6 months—5 years. Among children who subsequently were shown to have laboratory-confirmed influenza infections, only 28% of those hospitalized and 17% of those treated as outpatients had a discharge diagnosis of influenza.
Clinical definitions have performed poorly in some studies of older patients. A study of nonhospitalized patients aged 60 and older years indicated that the presence of fever, cough, and acute onset had a positive predictive value of 30% for influenza. Among hospitalized patients aged 65 years and older with chronic cardiopulmonary disease, a combination of fever, cough, and illness of <7 days had a positive predictive value of 53% for confirmed influenza infection. In addition, the absence of symptoms of influenza-like illness (ILI) does not effectively rule out influenza; among hospitalized adults with laboratory-confirmed infection in two studies, 44%—51% had typical ILI symptoms. A study of vaccinated older persons with chronic lung disease reported that cough was not predictive of laboratory–confirmed influenza virus infection, although having both fever or feverishness and myalgia had a positive predictive value of 41%. These results highlight the challenges of identifying influenza illness in the absence of laboratory confirmation and indicate that the diagnosis of influenza should be considered in patients with respiratory symptoms or fever during influenza season.
Hospitalizations and Deaths from Influenza
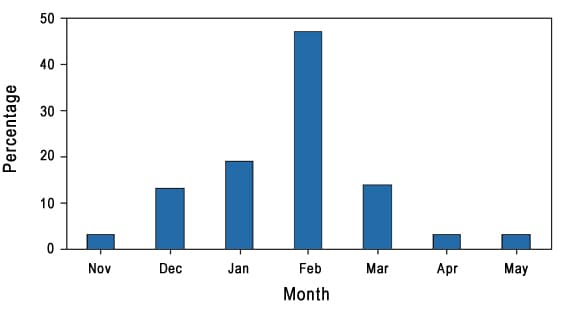
In the United States, annual epidemics of influenza typically occur during the fall or winter months, but the peak of influenza activity can occur as late as April or May (Figure 1). Influenza-related complications requiring urgent medical care, including hospitalizations or deaths, can result from the direct effects of influenza virus infection, from complications associated with age or pregnancy, or from complications of underlying cardiopulmonary conditions or other chronic diseases. Studies that have measured rates of a clinical outcome without a laboratory confirmation of influenza virus infection (e.g., respiratory illness requiring hospitalization during influenza season) to assess the effect of influenza can be difficult to interpret because of circulation of other respiratory pathogens (e.g., respiratory syncytial virus) during the same time as influenza viruses.
During seasonal influenza epidemics from 1979—1980 through 2000—2001, the estimated annual overall number of influenza-associated hospitalizations in the United States ranged from approximately 55,000 to 431,000 per annual epidemic (mean: 226,000). The estimated annual number of deaths attributed to influenza from the 1990—91 influenza season through 1998—99 ranged from 17,000 to 51,000 per epidemic (mean: 36,000). In the United States, the estimated number of influenza-associated deaths increased during 1990—1999. This increase was attributed in part to the substantial increase in the number of persons aged 65 years and older who were at increased risk for death from influenza complications. In one study, an average of approximately 19,000 influenza-associated pulmonary and circulatory deaths per influenza season occurred during 1976—1990, compared with an average of approximately 36,000 deaths per season during 1990—1999. In addition, influenza A (H3N2) viruses, which have been associated with higher mortality (54), predominated in 90% of influenza seasons during 1990—1999, compared with 57% of seasons during 1976—1990.
Influenza viruses cause disease among persons in all age groups. Rates of infection are highest among children, but the risks for complications, hospitalizations, and deaths from influenza are higher among persons aged 65 years and older, young children, and persons of any age who have medical conditions that place them at increased risk for complications from influenza. Estimated rates of influenza-associated hospitalizations and deaths varied substantially by age group in studies conducted during different influenza epidemics. During 1990--1999, estimated average rates of influenza-associated pulmonary and circulatory deaths per 100,000 persons were 0.4--0.6 among persons aged 0--49 years, 7.5 among persons aged 50--64 years, and 98.3 among persons aged 65 years and older.