
To determine appropriate influenza pandemic containment and mitigation measures, health authorities need to know the approximate case fatality ratio (CFR) for this new infection. We present four different methods for very provisionally estimating the plausible range of the CFR for symptomatic infection by this pandemic strain in developed countries. All of the methods produce substantially lower values (range 0.06% to 0.0004%) than a previously published estimate for Mexico (0.4%). As these results have many limitations, improved surveillance and serological surveys are needed in both developed and developing countries to produce more accurate estimates.
The first published estimate of the case fatality ratio (CFR) for those infected by the influenza A(H1N1)v pandemic strain was based on data from Mexico [1]. This work estimated the CFR to be 0.4% (range 0.3% to 1.5%) based on confirmed and suspected influenza A(H1N1)v-related deaths reported up to late April 2009. Since that date, the new pandemic strain has spread globally and new impact data are available, but we were unable to identify new estimates of the CFR in the literature. Yet this figure is critical if health authorities are to produce reasonable estimates of the likely impact of the pandemic in their particular countries. The estimated mortality burden is particularly useful for calibrating appropriate containment and mitigation measures that balance the likely health gains from interventions against their social and economic costs.
Methods
We considered four different ways to provide provisional estimates for plausible ranges of CFRs in developed countries for this pandemic.
Multiplier method
This method used confirmed deaths and cases reported to the World Health Organization (WHO), but with a range of multipliers for the latter to adjust for under-ascertainment. These multipliers were based on expert judgement that most symptomatic cases of the new pandemic involve relatively mild symptoms and that the great majority of cases were not being identified and reported. For example, spokespeople from the United States (US) Centers for Disease Control and Prevention (CDC) have announced “hundreds of thousands of cases that have occurred in the US” in late May and mid-June 2009 [2,3]. Similarly, one estimate for the United Kingdom was 30,000 cases in the community in May 2009 [4]. Regarding the choice of a multiplier to adjust data on laboratory-confirmed cases of pandemic influenza, we considered the above assessments, which are specific to the current pandemic, to be more informative than past experience with seasonal influenza, which only provides very broad estimates of a potential multiplier. For example, it has been estimated for seasonal influenza in the US that there are 2.3 influenza cases in the community for every outpatient consultation, and 84.1 for every case that is hospitalised (derived from Molinari et al. [5]). But during a pandemic, patients are encouraged to remain at home unless they have “severe illness” or are “at high risk for influenza complications”. Additionally, laboratory testing capacity can be quickly saturated in a pandemic and priority is given to those who require hospitalisation or are at high risk for severe disease [6]. These processes will tend to push the ratio of community cases to laboratory-confirmed cases upwards to the multiplier in the range of 10-30 that we judged reasonable for this analysis.
In the calculations we used WHO data for cumulative cases and deaths as of 26 June 2009 [7] for all member countries of the Organisation for Economic Cooperation and Development (OECD), but excluding data from Mexico. The reason for this exclusion was that the epidemic appeared to have started in Mexico and we were concerned about the quality and sensitivity of numerator data in the early stages of the epidemic there, i.e. when it was not recognised that the new pandemic strain was spreading.
Community survey method
This method used an estimate for community cases from a telephone survey done by the New York City Department of Health [8]. It reported that 6.9% of New Yorkers had symptoms of influenza-like illness (ILI) between 1 and 20 May 2009. The report on this survey did not publish confidence intervals, so we calculated these to be 5.6% to 8.5% (for the survey of 1,005 households). Furthermore, at the time of this survey, only 90% of the influenza samples tested in the city were of the current pandemic strain [9], and so we adjusted the CFR estimate accordingly by this proportion. We conservatively used the cumulative death toll for New York City at three weeks after the time period used in this survey (when it was n=12) to allow for a lag in illness progression and then in reporting fatalities to health authorities [10]. We identified that there were no pandemic influenza deaths prior to May [11] and the New York City population of 8,274,500 used in our calculations was that for 2007 [12].
Method extrapolating from seasonal influenza mortality
This method was based on evidence that the elderly population appear to have a relatively low mortality rate compared to other age groups in this pandemic. Data from Canada on hospitalisations and deaths [13] and US data indicate a median age of hospitalisation at 19 years and of death at 37 years [14]. Hence, we assumed that a CFR for seasonal influenza in the age group of under 65 year-olds could provide a crude approximation for the CFR of the new pandemic strain. To obtain this value we used the full range estimates that could be derived from a detailed US study [15] that used seven models for determining excess mortality attributable to influenza (Table 1).
Table 1. Estimates of annual seasonal influenza-associated deaths in the <65 year-old population with average results for the 1976-7 season through to the 2002-3 season* and calculated case fatality ratios 
Method extrapolating from a more ‘mature’ epidemic
This method was restricted to data from Canada and assumed that the epidemic there was relatively advanced in that the trend data for cases and hospitalisations were suggestive of a peak in early June with a subsequent waning of the epidemic in the following three weeks [17]. To calculate the CFR, we assumed that the epidemic in Canada was half complete in terms of cumulative deaths (with n=21 deaths confirmed as of 26 June [17]), which is possibly a conservative assumption given the low level of new hospitalisations in late June. We also assumed that the cumulative total of symptomatic cases would ultimately reach between 5% of the total population (which is within the range of seasonal influenza) and around 30% (which is approximately the value predicted by modelling for a pandemic with an R0 value of 1.5 [18] as estimated for the current pandemic using the Mexican data [1]).
Results
The four different methods produced a wide range of estimates for the CFR in developed countries, from 0.0004% to 0.06%, a range of 150-fold (Table 2). The ranges for each model overlapped with at least one other model. When these CFR estimates were applied to a country with a population of 10 million, that ultimately experienced a cumulative incidence of symptomatic infection with the pandemic strain of 30%, the total number of deaths would range from 12 to 1,800 (Table 2).
Table 2. Case fatality ratio for symptomatic infection with influenza A(H1N1)v pandemic strain in developed countries, estimated by four different methods 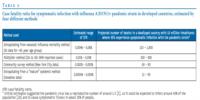
Discussion
All these estimated CFRs are substantially lower than the previously published estimate (0.4% for Mexico). They also differ markedly from the simplistic estimate that would be derived from using surveillance data available only for confirmed cases reported to WHO (i.e. of CFR = 0.29%, based on 110 deaths in 38,409 cases for the 29 OECD countries used in this analysis [7]). A low CFR would be consistent with the mild first wave seen in previous pandemics which caused widespread infection but low mortality [19]. It could also be related to the relatively young age of the majority of cases and the use of highly effective modern treatment for those who are seriously ill.
Although based on the most current data possible, all the methods used still have substantial limitations. The multiplier method merely relied on the judgement (from other experts as well as ours) of widespread and relatively mild disease that is not being reported. Nevertheless, the suggestion of widespread community spread in the US is broadly consistent with the community survey in New York City and another community survey in the US with around 6% cumulative incidence of ILI [14].
The New York City survey was limited by asking only about ILI that occurred during a 20-day period in May and by ignoring illness in April even though there were hospitalisations in New York City in that month. Therefore the method using this survey could have overestimated the CFR, although the opposite could have occurred if some of the reported ILI symptoms were due to other respiratory infections and allergic conditions such as hay fever.
The method that extrapolated from seasonal influenza mortality data in under 65 year-olds was limited in that it effectively considered no aspects of the epidemiology of the new pandemic influenza virus other than the age distribution, i.e. that it seems to affect younger age groups more than older age groups. Yet there is little information comparing the current pandemic strain with seasonal influenza strains in terms of mortality risk in this younger age group. Furthermore, the data from which the estimated range was derived may be outdated in that modern medical care has progressed since the early part of the period used in the particular US study [15] that the estimates were based on.
Although the Canadian epidemic appears to be waning, the method using the crude extrapolation of the course of this epidemic was very simplistic. Indeed, rather than being half complete, this epidemic wave could continue throughout the northern hemisphere summer and beyond.
These methods tended to focus on correcting for under-ascertainment of the denominator, yet there is also a potential bias from under-ascertainment of the numerator of the CFR. Particularly in the early stages of an epidemic there will be a lag in reported deaths and other severe outcomes. Sophisticated statistical methods have been proposed for obtaining adjusted CFR estimates using data from the early phase of an epidemic [20], and these result in adjustment for various time lags and an upward shift of the CFR. However, such adjustments would probably have little effect on the estimates presented in this article which are based on data from country epidemics which have progressed well beyond their early stages (e.g. the Canadian data). There is also the potential for under-recognition of deaths attributable to influenza in those with serious co-morbidities, but this can only be addressed by careful research studies and post-epidemic modelling to determine total excess deaths. Nevertheless, this bias might be relatively smaller in this pandemic where more deaths involve young people. Also, once the new influenza A(H1N1)v strain was recognised there is likely to have been increased sensitivity for diagnosing influenza-related deaths (at least in developed countries where hospitalisation is likely to precede influenza-related death).
All of the presented methods have limitations and could be refined using additional data to provide more robust estimates. Ultimately, such estimates require enhanced surveillance, outbreak investigations in a range of settings, and carefully designed population studies, ideally with serological testing [21]. Additionally, the ranges of CFRs for disadvantaged populations in developed countries and for most of the population in developing countries are likely to be much higher than those estimated here, given likely differences in disease transmission, co-morbidity, access to antivirals and standards of medical care.
Conclusion
We present several methods for provisionally estimating the plausible range for the CFR of the emerging influenza pandemic in developed countries. All methods used have significant limitations, but they collectively suggest that infection with this particular pandemic strain is likely to cause illness with a relatively low CFR compared to an earlier estimate and also to historical standards. A further reason for presenting this range of methods is to encourage data collection that can start to reduce the uncertainty around this important pandemic parameter.
Acknowledgements
Our thinking on this topic has been stimulated by conducting funded contract work for the New Zealand Ministry of Health, though this contract work was focused on evaluating potential interventions that related specifically to the New Zealand setting.